Oral Presentation Australasian Diabetes in Pregnancy Society and Society of Obstetric Medicine Australia and New Zealand Joint Scientific Meeting 2021
Comparing IADPSG and NICE diagnostic criteria for GDM in predicting adverse pregnancy outcomes (#3)
Background: The diagnostic criteria of GDM remains diverse across the world. In UK, National Institute for Health and Care Excellence (NICE) proposed a diagnostic criteria different from The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) criteria which adopted by the World Health Orgnaisation (WHO) in 2013. Our objective is to compare the NICE and IADPSG criteria in discriminating adverse pregnancy outcomes.
Methods: We performed a secondary analysis of data from 6397 participants of Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) study data from 5 of the 15 original study centres and compared the adverse pregnancy outcomes amongst participants who diagnosed as Group 1) normal glucose tolerance (NGT) by both the IADPSG and NICE criteria, Group 2) GDM by the IADPSG but NGT by the NICE criteria; Group 3) GDM by the NICE, but NGT by the IADPSG criteria and Group 4) GDM by both IADPSG and the NICE criteria.
Results: Among Hispanics, IADPSG criteria diagnosed more women with GDM than NICE criteria (19.5% vs 10.8 %, p<0.001) and performed better in the prediction of hypertensive disorders (gestational hypertension/pre-eclampsia), primary caesarean section, large for gestation age [LGA] (birth weight >=90th percentile), macrosomia (birth weight >=4 kg), adiposity (percentage of fat >=90th percentile) as well as neonatal hyperinsulinemia (umbilical cord serum C peptide level >=90th percentile) (Table 1).
On the other hand, among Asians, NICE criteria diagnosed more women with GDM (16.7% vs 13.8%, p<0.001) without identifying more women with adverse pregnancy outcomes. Among the Whites, IADPSG criteria can identify more women with LGA, while the NICE criteria identify more neonates with hyperinsulinemia (Table 1).
Conclusion: The result suggests that the IADPSG criteria may be more appropriate for Hispanics and Asians in the diagnosis of GDM.
Table 1 Comparisons of the incidences of neonatal outcomes by groups among each ethnicity
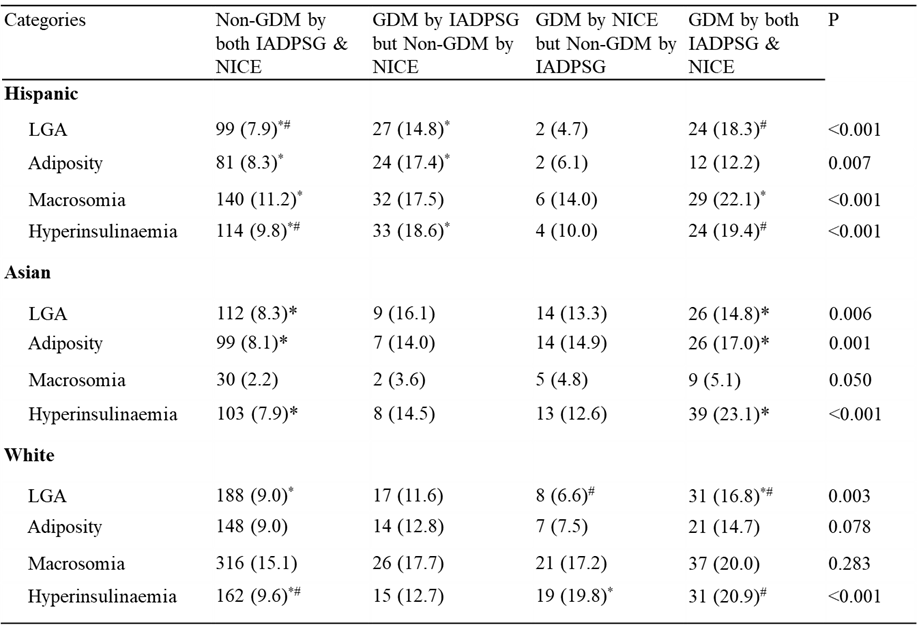
*# P<0.05